Physiology of Human Excretory System Parts and Functions Structure Organs
The Physiology of Human Excretory System involves the process of excretion of the waste products from the body. In this article we have described about the whole Physiology of Human Excretory System.
Function of Kidney | Kidney Structure | Structure of Nephron | Renal Corpuscle | Renal Tubule | Types of Nephron
Juxta Glomerular Apparatus | Mechanism of Urine Formation | Tubular Secretion | Concentration of Urine | Micturition
What is Excretion?
Excretion refers to elimination of principal products of metabolism except carbon dioxide i.e. removal of ammonia, urea, uric acid, creatinine, various pigments and inorganic salts. Different organs and systems like digestive system, respiratory system, excretory system and skin are involved in the process of excretion. Chiefly kidneys are main excretory organs.
Renal system constitute of :
- A pair of kidneys – production of urine.
- Ureters – transport urine to urinary bladder.
- Urinary bladder – store urine.
- Urethra – help in excretion of urine outside the body.
Physiology of Human Excretory System:-
Functions of kidney
The kidneys do the major function of the urinary system. The other parts of the system are mainly passageways and storage areas. It is important to known about kidney functions to understand the physiology of human excretory system. Functions of kidney are as follows:
-
Homeostatic function:
It maintains constancy of the interval environment of body by-
(a) Regulating blood ionic composition -Kidneys regulate the blood levels of several ions like Na+, K+, Ca++, Cl etc.
(b) Regulating blood pH – It maintain blood pH by excreting variables amount of H+ ion into urine and conserving H2CO3 in the blood.
(c) Regulating blood volume – It adjust blood volume by conserving or eliminating water in urine.
(d) Regulating blood pressure – It regulate blood pressure by secreting renin .
(e) Maintain blood osmolarity – By regulating loss of water and loss of solutes in the urine. Kidneys maintain relatively constant blood osmolarity 300 milli osmoles/liters.
-
Endocrine function:
It secretes:
(a) Erythropoietin hormone which stimulates production of RBC from stem cell.
(b) 25-Dihydroxycholecalciferol (active form of vitamin D), which helps to regulate calcium homeostasis.
(c) Renin from Juxta-glomerular cells in response to low BP.
(It converts angiotensinogen into angiotensin I which in presence of angiotensin converting enzyme is converted into angiotensin II which is a powerful vasoconstrictor and helps to maintain BP.)
-
-
Regulating blood glucose level:
Kidneys can also synthesize glucose from amino acid, glutamine etc.
-
Excreting waste and foreign substances:
By forming urine kidneys help to excrete wastes.
-
Regulating blood pressure:
It regulates blood pressure by secreting renin.
-
Thus all these functions of the kidney help to maintain Physiology of Human Excretory System.
Kidney structure
(Physiology of Human Excretory System)
It is very essential to know about the structure of the kidney otherwise Physiology of Human Excretory System can’t be understood.

physiology of human excretory system
- The kidneys are paired organs.
- Weighting 150 gm each in adults.
- They are located retro-peritoneal in the upper dorsal region of the abdominal cavity on either side of vertebral column.
- It is bean shaped organ approximately 10 cm long, 5 cm wide and 2.5 cm thick.
- Right kidney occupies slightly lower position due to pressure of liver on that side.
- The lateral border of each kidney is convex and its medial side is deeply concave.
- In the middle of the medial side there is depression leading to a hollow chamber called renal sinus through which blood vessels, nerves, lymphatic renal pelvis and ureter passes.
- Vertical section of kidney shows:
-
- Outer cortex : reddish in colour looks granular due to arrangements of nephrons. It forms shell-surrounding medulla.
- Inner medulla : is pale in colour. It contains 10 – 15 conical mass of tissues called pyramids whose bases are directed towards convex surface of the kidney. They terminate medially in the renal papillae. Papillae projects into calyces, such 10 – 15 minor calyces join to form two major calyces, which come out through pelvis of kidney to the widened end of the ureter.
Structure of nephron
To have a keen understanding of the Physiology of Human Excretory System, it is very essential to understand the fundamental unit of kidney.
Nephron is the basic functional unit of the kidney. There are about 1.2 million nephrons in each kidney, which drain into pelvis. Total length of nephrons is 45-65mm. Each nephron is formed by two parts:
- Malpighian or Renal corpuscle.
- Renal tubule.
Renal Corpuscle –
It is a rounded structure comprising glomerulus, surrounded by glomerular capsule also called as Bowman’s capsule.
Glomerulus–
It is a tuft of anastomosing capillaries. Blood enters the glomerulus through afferent arterioles and leaves it through efferent arterioles. Capillaries are made up of single layer of endothelial cells.
Structure of glomerular membrane
It is the membrane through which blood filters from capillaries into Bowman’s space and it is also called as filtration barrier. It is made up of three layers:
- Endothelial layer of capillaries: The endothelium is fenestrated i.e. contains holes of about 70-90 nm and is freely permeable to water, small solutes such as sodium, urea and glucose and even very small proteins but not all since this layer have negatively charged glycoproteins on their surface, which retard the filtration of large anionic proteins.
- Basement membrane: This is a porous matrix (pore size <8nm) of extra cellular proteins including collagen, laminin, fibronectin and other negatively charged proteins. It is an important filtration barrier to plasma protein. Unlike other basement membrane it is very thick.
- Visceral layer of Bowman’s capsule/ layer of podocytes.: It has special type of cells called podocytes, which have finger like projections. These projections interdigitate to cover the basement membrane and are separated by gaps called filtration slits. Each filtration slit is bridged by a thin diaphragm, which contains pores with dimensions of 25 nm. Therefore, filtration slit retard the filtration of some proteins and macromolecules that pass through endothelium and basement membrane.
Bowman’s capsule–
It is a cup shaped structure having two layers:
- Visceral layer – closely applied to the loops of capillaries from all sides.
- Parietal layer – form the outer layer having glomerulus and is continuous with epithelial lining of proximal tubule.
A space between visceral layer and parietal layer is called as Bowman’s space.
Renal tubule
The tubular portion of nephrons is the continuation of Bowman’s capsule.
It is made up of four parts:
- Proximal convoluted tubule (15 mm)
- Loop of Henle (14 – 26 mm)
- Distal convoluted tubule (5 mm)
- Collecting duct (20 mm)
Proximal convoluted tubule (PCT)
- The initial coiled, portion is called as pars convolute while distal portion is straight and is called as pars recta.
- The epithelial lining is continuous with the parietal layer of Bowman’s capsule.
- The apical surface has brush border due to presence of microvilli in order to increase the absorptive surface area.
Function:
- These cells take part in active reabsorption and secretion of some organic substances and ions.
- Glucose, amino acid, lactic acid, uric acid, ascorbic acid, phosphate, sulphate, potassium, calcium, sodium ions and water are reabsorbed while penicillin, histamine, creatinine and H+ are actively secreted.
Loop of Henle
It consists of
- Descending thin segment (DTS),
- Ascending thin segment (ATS)
-
Ascending thick limb (TAL)
The fluid in the descending limb runs toward renal pelvis and in ascending limb run towards cortex.
The DTS and ATS are made up of single layer of squamous epithelial cells which do not have brush border and have very few or no mitochondria so these are metabolically inactive and only passive transport process can take place in these segments.
The TAL has cuboidal epithelial cell layer with prominent brush border and has large number of mitochondria. Therefore, TAL has functions similar to that of PCT.
Function
- Water is reabsorbed from descending limb.
- Na, K and Cl ions are reabsorbed from ascending limb .
Distal convoluted tubule (DCT)
TAL is continuous with DCT. This tubule comes very close to its own glomerulus and establishes a close proximity to the afferent and efferent arteriole of the glomerulus.
At this point the cells of the tubule get modified and closely crowned together and called as Macula densa cells.
Function:
- DCT is an important site for active secretion of ions, acids etc.
- Na ions are actively reabsorbed and water is reabsorbed in presence of ADH and H ions are secreted actively.
Collecting duct (CD)
- The collecting duct, strictly speaking is not a part of nephron because it is derived from the ureteric buds. Depending upon the region where it is present, is divisible into three parts:
i) Cortical collecting duct.
ii) Outer medullary collecting duct.
iii) Inner medullary collecting duct.
- The last part of DCT and continuing collecting duct has two different types of cells:
i) Principal cell (P-cell):- They are abundant in number, and contains very few mitochondria. They have receptor for ADH & aldosterone hormone so increase the permeability for water & Na+.
ii) Intercalated cell (I- cell):- Few in number and have large number of mitochondria.
- They play role in maintaining blood pH by secreting H+ in the urine.
Types of nephron
(Physiology of Human Excretory System)
There are two types of nephrons cortical nephron and Juxta medullary nephron.
| Cortical nephron | juxtamedullary nephron | |
| Number of nephron | 80 – 85% | 15%. |
| Size and location of
glomeruli
|
Small size glomerulus in renal cortex
|
Large size, located at the
junction of cortex and medulla.
|
| Loop of henle | Short loop of henle may reach upto medulla.
In ascending limb ATS is Absent.
|
Long loop of henle goes deep into the medulla
Both ATS and TAL are present in ascending limb
|
| Vascular supply | Vascular supply is in the form
Of peritubular capillaries
|
It is in the form of vasa recta.
|
| Function | Mainly involved in the formation of urine
|
Involved in the concentration
of urine |
Thus this is all about the structural Physiology of Human Excretory System. Now we move toward information that enhance our knowledge about the Physiology of Human Excretory System.
Juxta glomerular apparatus (JGA)
(Physiology of Human Excretory System)
- It is a combination of specialized tubular and vascular cells located at the vascular pole where the afferent and efferent arterioles enter and leave the glomerulus.
- It is composed of three types of cells:
1. Juxta glomerular cells –
- These are specialized myoepithelial cells located in the media of afferent arterioles.
- They have well developed golgi apparatus, endoplasmic reticulum, mitochondria and ribosomes.
- They synthesize store and release an enzyme called renin.
- These cells act as baroreceptor as they respond to change in blood pressure and also monitor vascular volume.
- They are richly innervated with sympathetic fibers.
2. Macula densa cells –
- These cells refer to the specialized renal tubular epithelial cells near the vascular pole.
- These cells have prominent nuclei and golgi complex.
- They act as chemo receptors and are stimulated by decreased NaCl load in DCT, thereby cause increase renin release.
3. Extraglomerular Mesangial cells or Lacis cells –
- These are supporting cells of JGA and found between capillary loops.
- They are contractile in nature and play role in glomerular filtration by increasing or decreasing the surface area of filtration membrane.
Functions of Juxtaglomerular apparatus:
- Secretion of hormones – It secretes two hormone:
- Renin
- Prostaglandin
- Secretion of other substances – It also secretes cytokinins like interlukins-2 and tumor necrosis factor.
- Regulation of glomerular blood flow and glomerular filtration rate.
Mechanism of urine formation:
(Physiology of Human Excretory System)
Three processes are involved in the formation of urine:
1) Glomerular filtration – It is the function of renal corpuscle of nephrons.
2) Tubular Reabsorption
3) Tubular Secretion
Reabsorption and secretion are the function of tubular part of nephron. Both these process are together are called tubular transport process.
Glomerular filtration:
(Physiology of Human Excretory System)
Glomerular filtration is defined as the ultrafiltration of plasma from the glomerular capillaries into the Bowman’s capsule. It is the first step in the urine formation.
To understand this process this section is divided into following sub headings:
- Characteristics of filtration membrane.
- Composition of glomerular filtrate.
- Dynamics of glomerular filtration.
- Glomerular filtration rate (GFR)
- Filtrations fraction.
- Factors affecting glomerular filtration.
- Regulation of glomerular filtration.
- Measurement of glomerular filtration.
1. Characteristics of filtration membrane:
Filtration membrane consists of three layers: capillary endothelium, glomerular basement membrane and visceral layer. The characteristic features of the membrane are:
1) It is highly permeable to water and to water soluble substances due to its porous nature.
2) This membrane also exhibits high degree of selective permeability which depends upon-
a) Pore size –
- Pore size of endothelial layer is 70 –90nm , of basement membrane is 8nm and of visceral layer is 25 nm. Therefore,
- Molecules less than 4 nm in size can freely pass.
- Molecules with diameter more than 8nm are not filtered at all.
- Filtration of molecules having diameter between 4nm –8nm is inversely proportional to their diameter.
b) Electrical charge –
This membrane is negatively charged due to presence of glycoproteins rich in silica acid. Therefore the negatively charged molecules are less permeable than neutral and positive charged molecules. This is the reason that albumin, although has 7nm molecular diameter, is not filtered.
2. Composition of glomerular filtrate :
It is similar to plasma composition except that it is devoid of cells and proteins. The composition may alter in some diseases due to alteration in permeability of membrane. For example in glomerular disease the negative charge of membrane is lost and protein filters across membrane and appears in the urine (Proteinuria / albuminuria) in significant amount.
3. Glomerular filtration rate (GFR):
The total quantity of filtrate formed in all the nephrons of both kidney in the given unit time is called as glomerular filtration rate (GFR).
The normal value of GFR in an average man is 125ml/min or 180 L/day. It is directly proportional to the surface area but in women it is 10% lower than in man. After age of 30year, GFR declines with age.
4. Dynamics of glomerular filtration:
The forces that determine the filtration of plasma are similar to the forces, which determine the absorption of fluid in interstitial space through capillaries.
GFR is the product of filtration coefficient and net filtration pressure.
GFR = Kf x Net filtration pressure.
Where, Kf is filtration coefficient, which depends upon the glomerular capillary membrane permeability and the surface area of filtration membrane and is equal to 12.5. Net filtration pressure is the difference of the forces that favours the filtration and the forces that opposes the filtration.
Basically four forces (Starling forces) act at the filtration membrane (Fig. 10)
- Hydrostatic pressure in glomerulus (PG) = 45 mm Hg.
- Hydrostatic pressure in Bowman’s space (PB) = 10 mm Hg.
- Oncotic pressure in glomerular capillaries (πG) = 25 mmHg
- Oncotic pressure in Bowman’s space (πB), which is taken as 0 as it does not contain proteins.
PG and πB favours filtration while Pb and πG opposes the filtration
Net filtration pressure = (PG + πB) – (PB + πG)
So, GFR = Kf x [(PG + πB) – (PB + πG)]
= 12.5 x (45 + 0 – 25 – 10)
= 12.5 x 10
= 125 ml / min
5. Filtration fraction (FF):
It is the fraction of plasma that flows through kidneys get filters at glomerulus into Bowman’s space.
GFR 125
FF = 0.16 – 0.22
RPF = 620 – 700
= 16 % – 22 %
Therefore, filtration fraction is 16 % – 22 % of RPF i.e., only 16 % – 22 % of plasma, that flows through kidneys, filters at glomerulus.
6. Factors affecting Glomerular Filtration Rate:
- GFR decreases with advancing age due to decrease in renal plasma flow, cardiac output and renal tissue mass.
- GFR change with Renal blood Flow in linearity.
- Hydrostatic pressure in glomerulus – If it increases GFR also increases.
- It increases in afferent arteriolar dilatation and efferent arteriolar constriction.
- It decreases with decreased arterial pressure, afferent arteriole constriction and efferent arteriole dilatation.
- Oncotic pressure in Glomerulus (πG) –
- Increase in it results in decrease in GFR
- Increase in Oncotic pressure in Glomerulus is seen in hyperproteinemia e.g. dehydration.
- Decrease in Oncotic pressure in Glomerulus is seen in hypoproteinemia e.g. severe anaemia and nephrotic syndrome
- Hydrostatic pressure in Bowman’s space (PB) –
With increase in it, GFR decreases e.g. obstruction to urine flow i.e. in ureteric calculus.
- Membrane permeability – The permeability of glomerular membrane increases in its infection as in glomerular nephritis and decreases when it becomes thick as in diabetes mellitus.
- Surface area of filtration membrane – Greater the surface area more will be the GFR while small surface area reduces GFR.
7. Regulation of GFR:
Since the same regulatory mechanism affects both GFR and RBF. Before discussing various regulatory mechanisms, it is essential to understand the relationship between changes in afferent arteriole and efferent arteriole with RBF and GFR
- Constriction of afferent arteriole decreases both RBF and GFR without charges in filtration fraction.
- Dilatation of the afferent arteriole increases both RBF and GFR without charges in filtration fraction.
- Constriction of efferent arteriole decreases the RBF but increases GFR so also filtration fraction.
- Dilatation of efferent arteriole increases RBF and Decreases GFR and filtration fraction.
The mechanisms that regulate RBF and GFR are:
- Auto regulation
- Hormonal regulation
- Nervous regulation
Auto-regulation of GFR and RBF:
(Physiology of Human Excretory System)
The renal blood flow (RBF) and the glomerular filtration rate (GFR) remain constant over a wide range of renal arterial pressures, 80-200mm Hg. This occurs due to an intra-renal mechanism known as auto-regulation.
Mechanism of auto-regulation:
Two mechanisms are considered responsible for autoregulation of RBF and GFR:
- Myogenic mechanism: It is related to an intrinsic property of vascular smooth muscle, the tendency to contract when it is stretched. Thus, when renal arterial pressure is raised, the afferent arterioles are stretched followed by constrict.
Increase in vascular resistance balance the effect of increased arterial pressure and there by maintains a constant RBF and GFR.
- Tubuloglomerular feedback (TGF) mechanism:
Tubulo-glomerular feedback (TGF) mechanism is based on the NaCl concentration of tubular fluid. It involves a feedback loop which operates as:
Physiological significance: Auto-regulation of GFR and RBF is an effective mechanism for uncoupling renal function from fluctuation in arterial pressure and maintain fluid and electrolytic balance.
Special features of auto-regulatory mechanisms
- Auto-regulation mechanisms do not work when the mean arterial blood pressure falls below 80 mm Hg or increases more than 200 mm Hg.
- Auto-regulation is not a perfect mechanism.
- Several hormones and other factors can change RBF and GFR in spite of auto-regulatory mechanisms.
Hormonal regulation:
(Physiology of Human Excretory System)
Both GFR and RBF are also influenced by hormones described as:

- Decrease in GFR &RBF by Vasoconstrictors-
- Nor epinephrine
- Angiotensin II
- Endothelin
- Increase in GFR & RBF by Vasodilators-
- Prostaglandins (no effect on GFR)
- Nitric oxide
- Bradykinin
- Dopamine
- Histamine
Nervous regulation:
(Physiology of Human Excretory System)
Kidneys were supplied by sympathetic fibres from T12 – L2 segments.
- At rest, sympathetic stimulation is moderately low.
- The afferent and efferent arterioles are dilated and renal auto-regulation, of GFR prevails.
- With moderate sympathetic stimulation, both afferent and efferent arteriole constrict to the same degree, decreasing GFR and RBF slightly.
- With greater sympathetic stimulation, during exercise and haemorrhage, vasoconstriction of afferent arteriole predominate, as a result, blood flow into glomerular capillaries is greatly decreased and GFR drops.
8. Measurement of GFR –
GFR can be measured by renal clearance of inulin, urea and creatinine.
Tubular transport process:
Glomerular filtrate formed per day is about 180 L and only 1.5 L is excreted in the form of urine. That is, 99% of filtered water and many useful substances are reabsorbed. The different segments of tubule like PCT, Loop of Henle, DCT and Collecting duct determines the composition and volume of urine by the process of selective reabsorption and selective secretion of water and solutes.
- General Consideration:
- Transport pathways and mechanisms across Tubular cell membrane In renal tubule, substances can be transported by two pathways
(i) Paracellular pathway: Transport between the cells through tight junctions.
(ii) Transcellular pathway: Transport across the cell. It is a two-step process.
The substances can be transported as:
a) Active transport process
b) Passive transport process– Diffusion, facilitated diffusion and solvent drag.
Selective re-absorption:
(Physiology of Human Excretory System)
The tubular cell reabsorbs the substances present in glomerular filtrate according to the need of the body. So the tubular reabsorption is selective reabsorption.
The various substances are classified into three categories:
1. High threshold substance –
- The substances like glucose, amino acids and vitamins are completely reabsorbed.
- They do not appear in the urine.
- These substances can reappear in urine only when their concentration in plasma is very high or in renal disease when they are not re-absorbed.
2. Low threshold substance –
- The substances are reabsorbed in little extent. eg urea, uric acid and phosphate
- These appear in urine even under normal conditions.
3. Non-threshold substance –
The metabolic end products are not reabsorbed and are excreted in urine irrespective of their concentration in plasma. eg creatinine
Differant ways of renal reabsorption:
- By glomerular filtration only, e.g. Inulin
- By glomerular filtration plus partial reabsorption, e.g. urea.
- By glomerular filtration plus complete reabsorption, e. g. Glucose
- By glomerular filtration plus partial secretion, e.g. PAH
- By glomerular filtration plus tubular reabsorption and secretion, e.g. K+.
- By only secretion, e.g. organic compound bound to proteins.
Quantification of renal tubular transport:
(Physiology of Human Excretory System)
1. Filtered load(Fo):
Amount of substance entering the tubule through glomerular filtration per unit time.
Fo = GFR x Px
2. Excretion rate (Eo):
It is the amount of substance that appear in the urine per unit time.
E o = V x Ux
V – Urine flow rate
U x – Concentration of substance in the urine.
3. Reabsorbtion rate (R):
The rate at which a particular substance is reabsorbed.
R = Fo – Eo
4. Secretion rate (S):
The rate at which substance is secreted from peritubular capillaries into the tubule. S = Eo – Fo
5. Tubular transport maximum:
The renal active transport system have a maximal rate or Transport maximum (Tm) at which they can transport particular solute. The transport system, in turn, depends upon the carrier substance or enzyme.
Tubular transport maximum (Tm for that solute) is the maximum rate at which a substance is reabsorbed or secreted.
Thus the amount of a particular substance transported is proportionate to the concentration of that solute but after certain limit, when that carrier becomes saturated then no amount of solute is transported.
Reabsorbed substances that have (Tm) are glucose, amino acids, uric acid, albumin etc. Secreted substances that have (Tm) are PAH, penicillin, certain diuretics, vitamins etc.
Transport across different segments of nephrons:
(Physiology of Human Excretory System)
-
Proximal convoluted tubule
The largest amount of solute and water reabsorption occurs in PCT.
Substances reabsorbed:
- PCT reabsorbed approximately 67% of the filtered water, Na+, Cl-, K+ and other solutes like Ca++, Mg++ and urea..
- Reabsorbtion of Glucose, amino acids and vitamins are 100% while that of HCO3– is 80-90%.
Substances secreted: H+, PAH, drugs, creatinine etc.
Mechanism
- Normally, filtered glucose, amino acids, lactic acid, water-soluble vitamins, and other nutrients are not lost in the urine.
- They are completely reabsorbed in the first half of the proximal convoluted tubule (PCT) by Na+ symporters located in the apical membrane.
- Another secondary active transport process the Na+ /H+ antiporters, carry filtered Na+ down its concentration gradient into a PCT cell in the exchange of H+ which is secreted into tubular fluid.
- Besides achieving reabsorption of sodium ions, the Na+ symporters promote osmosis of water and passive reabsorption of other solutes. As water leaves the tubular fluid, the concentration of the remaining filtered solutes increase.
- In the second half of the PCT, electrochemical gradients for Cl- , K+ , Ca2+ , Mg2+ , and urea promote their passive diffusion into peritubular capillaries via both paracellular and transcellular routes. Among these ions, Cl- is present in the highest concentration.
- Each reabsorbed solute increases the osmolarity, first inside the tubule cell, then in interstitial fluid, and finally in the blood. Water thus moves rapidly from the tubular fluid, via both the paracellular and transcellular routes, into the peritubular capillaries and restores osmotic balance. Cells lining the proximal convoluted tubule and the descending limb of the loop of Henle are especially permeable to water.
Loop of Henle:
The LH reabsorbs about:
- 20-30% of the filtered Na+, K+, Ca2+;
- 10 – 20% of the filtered HCO3;
- 35% of the filtered Cl-; and
- 15% of the filtered water.
Distal Convulated Tubule:
The distal convoluted tubule reabsorbed Filtered NaCl (7%) and water (8-17%) while secrete K+ and H+.
- Early DCT – Reabsorbs Na+, Cl-, and Ca++ but is impermeable to water like ALH.
- Fluid enters the distal convoluted tubules (DCT) at a rate of about 25mL/min.
- The DCT also is the major site where parathyroid hormone (PTH) stimulates reabsorption of Ca+.
- Principal cell –
It causes reabsorption of
- Na+ actively across basolateral surface with help of Na +K+ ATPase and passively across apical membrane,
- Cl- passively through paracellular route,
- Water only in presence of ADH.
- It causes secretion of K+ via Na +- K + ATPase across basolateral membrane and which diffuses passively across apical membrane.
- Intercalated cell – It reabsorbs K+ by H+ – K+ ATPase in the apical membrane and secretes H+ by H+ ATPase.
Transport of various substances across different segments of nephrons:
(Physiology of Human Excretory System)
Reabsorption of Sodium:
From the thick ascending limb (TAL) sodium is actively pumped out into the outer medullary interstitium. It enters the outer medullary descending thin segments (DTS). This results in recycling of Na+ in the long loops of the juxtamedullary nephrons. The recycling causes accumulation of Na+ in the interstitium of the renal medulla.
Reabsorption of water:
Rapid diffusion of water across the cell membrane occurs through water channels made up to proteins called Aquaporins. Renal handling of water by different segments of renal tubule is as follows:
- From PCT: Passive reabsorption (67 %).
- From Loop of Henle:
- Descending thin segment (DTS): Passive reabsorption (15 %)
- Ascending thin segment (ATS): Impermeable
- Thick ascending limb (TAL): Impermeable
- From Distal tubule and collecting duct: (8 to 17 %)
- Early DCT: Impermeable
- CD: Reabsorption is ADH dependent
- OMCD: Reabsorption is ADH dependent
- IMCD: Reabsorption is ADH dependent
80% out of the total amount of water reabsorbed from the nephron, irrespective of the body water balance.
Regulation of NaCl and water absorption
Hormonal regulation.
- Various hormones including angiotenisn II, aldosterone, ADH, ANP, epinephrine and nor epinephrine (released from sympathetic nerves) and dopamine, regulates NaCl reabsorption.
- ADH is the only major hormone that directly regulates the amount of water excreted by kidney.
Glomerulotubular balance (GTB) –
As GFR increases, the tubular reabsorption of solutes and water increases in PCT due to glomerulotubular balance (GTB). This mechanism in the proximal tubule maintains reabsorption at a constant fraction (2/3 or 67 % of the filtered Na+ and H2O). It is because of oncotic pressure in the peritubular capillaries.
When GFR increases, more amount of plasma proteins accumulate in the glomerulus. Consequently, the oncotic pressure increases in the blood by the time it reaches to the efferent arteriole and peritubular capillaries. The elevated pressure in the capillaries increases re-absorption of sodium and water from PCT.
Effects of ECF volume on proximal tubular re-absorption.
- ECF volume contraction increases re-absorption.
- ECF volume expansion decreases re-absorption.
Re-absorption of glucose:
- Glucose is freely filtered into glomerular filtrate. Filtration load (Fo) increase is direcly proportional to the plasma glucose concentration (PG).
- PCT completely reabsorbed all filtered glucose. The transport mechanism occurs in two steps:
- From lumen into cell via secondary active transport processes– Glucose binds with carrier protein, Sodium – Glucose transporter (SGLUT), located at the apical membrane.
- From cell into the intercellular space via facilitated diffusion – GLUT-2 and GLUT-1 are carrier for this transport.
Characteristic features of glucose re absorption:
- Glucose is reabsorbed by transport maximum process. It is depend upon the number of Na+ glucose transporter.
- The glucose reabsorbtion and excretion processes are function of the plasma glucose titration curve:
- Increase in the plasma glucose concentration result in progressive linear increase in the filtered load.
- At low plasma glucose concentration glucose reabsorption is 100% i.e. no amount of glucose appears in urine. In this region, line of reabsorption is same as that of filtration.
- When plasma glucose concentration increase above 180-200 mg the glucose reabsorption is incomplete and glucose appears in urine (Glycosuria).
- The plasma glucose concentration at which glucose appears in urine is called as Renal Threshold for glucose. It is 200 mg % of arterial plasma and 180 mg% of venous plasma.
- Tm for glucose is 375 mg/min i.e. after this plasma glucose concentration level reabsorption rate become constant and is independent of PG.
- It is between plasma glucose concentration 180mg % and 350 mg% i.e. the predicted renal threshold for glucose is 300mg.
Re-absorption of proteins, peptides and amino acids:
- Like glucose, peptides and amino acids filter across glomerular membrane and are 100 % reabsorbed while proteins are not filtered.
- The small amount of protein that is present in the urine usually comes from the tubular shedding.
- Normal amount of protein in urine is 150 mg in a day.
- Re-absorption of amino acids is via secondary active transport process and facilitates diffusion just like that of glucose.
Reabsorption of Urea:
- The amount of urea filtered by glomerular capillaries varies with protein intake.
- PCT reabsorbs 5% of filtered urea passively.
- DTS and ATS, CD, OMCD are totally impermeable to urea.
- IMCD is permeable to urea so reabsorbs large amount of urea in the effect of ADH.
Reabsorbtion of uric acid:
Urate is freely filtered by the glomerular capillaries.
Mechanisms:
- Passive reabsorption through paracellular pathway.
- Secondary active transport through transcellular pathways involves two steps–
a) Across apical membrane- It enters the cell by counter transport with intracellular ions like Cl-, HCO3- etc.
b) Across basolateral membrane- The urate moves out using another anion exchanger.
Tubular Secretion:
(Physiology of Human Excretory System)
Tubular secretion is the transfer of materials from peritubular capillaries to the renal tubular lumen. The substances secreted into the tubular fluid for removal include:
- Potassium ions (K+)
- Hydrogen ions (H+)
- Ammonium ions (NH4+)
- Creatinine
- Urea
- Some hormones
- Some drugs (e.g., penicillin)
It is the tubular secretion of H+ and NH4+ from the blood into the tubular fluid that helps to keep blood pH at its normal level this is also a respiratory process.
The substance that remains in the collecting duct of the kidneys following reabsorption is better known as urine.
Urine leaves the kidney though the ureter following secretion.
Mechanism
The mechanisms by which secretion occurs are:
- Passive diffusion– The movement of molecules from the peritubular capillaries to the interstitial fluid within the nephron.
- Active transport– The movement of molecules via ATPase pumps that transport the substance through the renal epithelial cell into the lumen of the nephron.
Hormonal regulation of tubular re-absorption and tubular secretion:
(Physiology of Human Excretory System)
Four hormones affect the extent of Na+, Cl-, and water re-absorption as well as K+ secretion by the renal tubules. The most important hormonal regulators of electrolyte re-absorption and secretion are
Angiotensin II-
- Causes vasoconstriction of the afferent arterioles leading to decrease GFR.
- Enhances reabsorption of Na+, Cl-, and water in the proximal convoluted tubule by stimulating the activity of Na+ /H+ antiporters.
- Stimulates release of aldosterone hormone from adrenal cortex that in turn, stimulates the reabsorb more Na+ and Cl- and secrete more K+.
- All these three mechanisms ultimately result in increase in blood volume.
ADH-
- Posterior pituitary releasesAntidiuretic hormone Antidiuretic hormone (ADH or Vasopressin).
- It regulates facultative water reabsorption.
- A second powerful stimulus for ADH secretion is a decrease in blood volume, as occurs in hemorrhage or severe dehydration.
- In the pathological absence of ADH activity, a condition known as diabetes insipidus, person may excrete up to 20 liters of very dilute urine daily.
Aldosterone-
- It stimulates the reabsorb more Na+ and Cl- and secrete more K+.
Atrial natriuretic peptide (ANP)-
-
- It plays a minor role in inhibiting both electrolyte and water reabsorption.
- A large increase in blood volume promotes release of atrial natriuretic peptide (ANP) from the heart.
- Although the importance of ANP in normal regulation of tubular function is unclear,It can inhibit reabsorption of Na+ and water in the proximal convoluted tubule and collecting duct.
- ANP also suppresses the secretion of aldosterone and ADH.
- These effects increase the excretion of Na+ in urine (natriuresis) and increase urine output (diuresis), which decreases blood volume and blood pressure.
Concentration of urine
(Physiology of Human Excretory System)
The kidney can excrete urine as dilute as 50 mOsm/L and as concentrate as high as 1200-1400 mOsm/L depends on water intake . The kidney can excrete large volume or small volume of urine without affecting the rate of solute excretion.
The loop of Henle of juxta medullary nephrons is the apparatus that allows the nephron to concentrate urine. It is a countercurrent multiplier system in which fluids move in opposite directions through side‐by‐side, semi‐permeable tubes.
Active and passive mechanisms are involve in transportation of substances, from one tube to the other. The movement of the transported substances up and down the tubes results in a higher concentration of substances at the bottom of the tubes than at the top of the tubes.
Descending limb:
- It is permeable to H 2O, so H 2O diffuses out into the surrounding fluids.
- It is impermeable to Na +and Cl –.
- Thus ions are not pump out and remain inside the loop.
- As the fluid continues to travel down the descending limb of the loop, it becomes more and more concentrated. This occurs due to diffusion of water outside.
- Thus, Maximum concentration occurs at the bottom of the loop.
Ascending limb:
- It is impermeable to water.
- Na +and Cl – , by active transport.
- They are pump out into the surrounding fluids.
- As fluid travels up the ascending limb, it becomes less and less concentrated because Na +and Cl – are pumped out.
- At the top of the ascending limb, the fluid is only slightly less concentrated than at the top of the descending limb.
- In other words, there is little change in the concentration of the fluid in the tubule as a result of traversing the nephron loop.
Collecting tubule:
- Fluid at the top of the collecting duct has a concentration of salts equal to that of at the beginning of the nephron loop. (some water is reabsorb in the DCT).
- As the fluid descends the collecting duct, the fluid is expose to the surrounding salt gradient establish by the nephron loop.
- Without ADH, the collecting duct is impermeable to H 2
- Urea recycling from the inner medullary collecting ducts is the process that contributes to establishment of hyperosmotic medulla.
- Two outcomes are possible:
- If water conservation is necessary, ADH stimulates the opening of water channels in the collecting duct, allowing H 2O to diffuse out of the duct and into the surrounding fluids. As a result formation of concentrated urine occurs.
- Similarly, if water conservation is not necessary. The ADH is not secrete. As a result allowing H2 to remain in the duct.
- The result is dilute urine.
Vasa Recta:
-
- The vasa recta deliver O 2and nutrients to cells of the nephron loop. The vasa recta, like other capillaries, is permeable to both H 2O and salts.
- It acts as a counter-current multiplier system as the vasa recta descends into the renal medulla, water diffuses out into the surrounding fluids, and salts diffuse in. When the vasa recta ascend, the reverse occurs.
- As a result, the concentration of salts in the vasa recta is always about the same as that in the surrounding fluids, and the salt gradient established by the nephron loop remains in place.
- It has two main features :
- Slow blood flow
- The vasa recta act as a counter current exchanger to minimize washout of solutes from the medullary interstitium. This is due to the U shape of vasa recta capillaries.
Thus this is all about the functional aspect of Physiology of Human Excretory System.
Micturition
(Physiology of Human Excretory System)
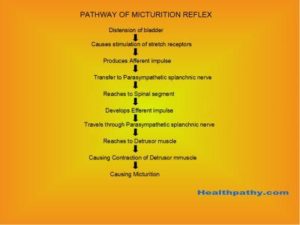
It is a complete autonomic spinal reflex through which urine is void from urinary bladder. Higher centers in the brain facilitate or inhibit the process of micturition.
Conduction of urine: It involves-
Kidney- Chiefly, involved in the formation of urine. Urine from the collecting duct enters into renal pelvis.
Ureters- They conducts the urine from the renal pelvis to the bladder through peristalsis.
Urinary bladder- It is a muscular bag that holds urine.
Urethra- It excrete urine outside the body.
Micturition involves two main steps:
- The tension in the wall of the bladder rises above threshold level.
- Nervous Reflex (micturition reflex) at 150-200 ml of urine volume.
Generation of peristalsis:
- In the renal pelvis there are “electrical pacemaker” cells that initiate peristaltic waves in the smooth muscle sheaths of the ureteral wall.
- The distension of pelvis stimulate the pacemaker.
- The movement of the peristalic wave is about 2‐6 cm/sec, traveling from its origin at the pelvis down to the bladder.
Parasympathetic stimulation increases peristaltic movement while sympathetic stimulation decrease it.
The smooth muscle of the bladder called Detrusor muscles which can increase the pressure in the bladder when contracted.
The Internal sphincter which is under control of involuntary nervous system (Hypogastric nerve) and can control urination.
Urethra pass through a layer of voluntary skeletal muscle called the external sphincter which is under control of voluntary nervous system (Pudendal nerve) and can control urination.
Pathway of micturition reflex:
(Physiology of Human Excretory System)
First of all we want to thank all our readers who are believing us. We hope you will also love this article medical notes on Physiology of Human Excretory System Parts and Functions Structure Organs too. If you like this article Physiology of Human Excretory System pls mention in comment box and like our facebook page also. Thank you.
Also Read:-
Information about digestive system Digestion process
Classification of Fracture | complete notes
Role of Community Medicine in Homoeopathy
Like us and Follow us on
facebook-
Healthy Life Tips
Twitter-
Healthpathy