Structural Determinants of Health
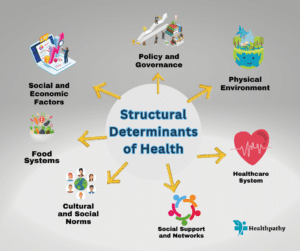
Health is a complex interplay of various factors that goes beyond individual behaviors and genetics. Among these factors, structural determinants of health play a pivotal role in shaping populations’ health status and well-being. These determinants encompass the societal, economic, environmental, and cultural conditions that individuals are born into, live within, and interact with throughout their lives. Understanding these determinants is crucial for formulating effective public health strategies and addressing health disparities.
Social and Economic Factors
Socioeconomic status (SES) is a significant structural determinant that strongly influences health outcomes. People with higher SES often have greater access to quality education, better job opportunities, and improved living conditions. Income inequality, a facet of SES, also impacts health. Countries with higher income inequality tend to experience worse health outcomes, even among affluent individuals.
Access to education is another vital determinant. Education equips individuals with the knowledge and skills necessary to make informed health decisions. Moreover, education correlates with employment opportunities, leading to improved financial stability and better access to healthcare.
Physical Environment
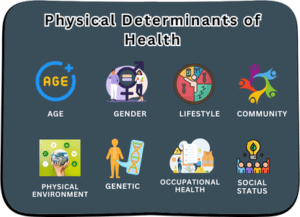
The physical environment in which individuals reside has a substantial impact on their health. Inadequate housing, characterized by overcrowding and poor sanitation, can lead to the spread of diseases and mental health issues. Neighborhood conditions, including the presence of green spaces, safe streets, and recreational facilities, influence physical activity levels and overall well-being.
Air and water quality are also critical. Exposure to pollutants can result in respiratory illnesses, cardiovascular diseases, and other adverse health outcomes. Marginalized communities often bear the brunt of poor environmental conditions, exacerbating health disparities.
Healthcare System
The healthcare system plays a crucial role in determining health outcomes. Access to healthcare services, including preventive care and timely treatment, is essential for maintaining health and managing chronic conditions. However, disparities in healthcare access persist based on race, ethnicity, gender, and socioeconomic background.
The quality of healthcare services is equally significant. Inequities in the distribution of healthcare resources and facilities can result in suboptimal care for marginalized populations. Addressing these disparities requires not only improving access but also ensuring that healthcare services are of high quality across all communities.
Social Support and Networks
Strong social networks and social support contribute to better health outcomes. Having a supportive community can reduce stress, promote mental well-being, and encourage healthy behaviors. Social cohesion, characterized by trust and a sense of belonging, has been linked to improved overall health.
Community resources and support systems are instrumental in providing assistance to vulnerable populations. Programs that foster social engagement and offer resources like childcare, transportation, and counseling can help alleviate the impact of structural disadvantages on health.
Food Systems
Food accessibility and quality significantly impact health. Limited access to nutritious foods can lead to poor dietary habits, contributing to chronic diseases like obesity and diabetes. Food deserts, areas with limited access to affordable, healthy food options, disproportionately affect low-income neighborhoods.
The marketing and availability of unhealthy foods also play a role in shaping dietary choices. Aggressive marketing of sugary and processed foods can influence consumer preferences and contribute to unhealthy eating patterns.
Cultural and Social Norms
Cultural beliefs and social norms influence health behaviors and outcomes. For example, certain cultural practices may affect individuals’ willingness to seek medical care or engage in preventive measures. Gender norms can also shape health behaviors, impacting reproductive health and mental health seeking.
Stigmatization of specific health conditions, such as mental illnesses or certain infectious diseases, can deter individuals from seeking care and support. Addressing these norms and reducing stigma is crucial for promoting equitable health outcomes.
Policy and Governance
Government policies have a profound impact on structural determinants of health. Education, income support, housing, and healthcare policies can exacerbate or mitigate health disparities. Social and economic policies that promote income equality, affordable housing, and accessible healthcare can significantly improve population health.
Collaboration between different sectors, including public health, education, housing, and social services, is essential for addressing structural determinants. A holistic approach that involves policy changes, cross-sector partnerships, and community engagement is necessary for meaningful progress.
Intersectionality of Structural Determinants
Structural determinants of health are interconnected and often intersect. Individuals experiencing multiple disadvantages due to factors like race, gender, and socioeconomic status face compounded health risks. These intersecting disadvantages can lead to greater health disparities and necessitate comprehensive interventions that address multiple determinants simultaneously.
Examples of Successful Interventions (Structural Determinants of Health)
Numerous interventions have demonstrated the potential for positive change in addressing structural determinants. Community-based programs that provide education, job training, and access to social services have shown success in improving health outcomes for marginalized populations. Additionally, policy changes, such as minimum wage increases and expansion of Medicaid, have led to improved access to resources and healthcare services.
Challenges and Future Directions
Implementing changes to address structural determinants of health is not without challenges. Resistance to policy changes, limited funding, and the complexity of addressing multiple determinants simultaneously can hinder progress. Longitudinal research is needed to measure the long-term impacts of interventions and ensure their sustainability.
Summary:
Understanding and addressing the structural determinants of health is crucial for achieving health equity and improving the well-being of populations. By recognizing the interconnectedness of social, economic, environmental, and cultural factors, we can develop comprehensive strategies that create lasting positive impacts on public health. It’s time to collaborate across sectors, advocate for policy changes, and empower communities to create a future where everyone has the opportunity to lead a healthy life.
Related Articles:

Follow us: Structural Determinants of Health





